You are here: vision-research.eu » Vision Research » Vision in the European Focus » 2014 » Pioneering experiments in the living eye
Pioneering experiments in the living eye

The light sensitive tissue of the human eye, the retina, is lined by roughly 130 Million photoreceptor cells. Scientists at the University of Bonn, University of California, Berkeley and University of Alabama at Birmingham were now able to target and stimulate individual photoreceptors – cell by cell – for the first time. The ground-breaking research promises new insights into how the brain transforms retinal images to visual perception. Also, single photoreceptor function and dysfunction in retinal disease and possible pharmaceutical intervention can now be studied on single cell level. The work is published in the April 16th issue of “The Journal of Neuroscience”.
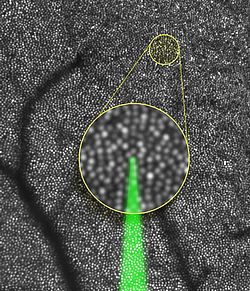
How visual perception arises from the activity of each photoreceptor cell in the retina is an important question in neuroscience, yet it is difficult to study in vivo. A team of German and American scientists have now developed a technical solution to approach this question directly. Using an adaptive optics scanning laser ophthalmoscope they were able to stimulate single cone-photoreceptors in the living eye and record perceptual responses from tested subjects. They found that it is sufficient to drive visual perception when only a single cell is activated, after a given intensity threshold was reached. Furthermore, single cones presented a remarkable variability in terms of their sensitivity to detect light. This was even measurable across the diameter of each cell. “We were able to show that perception thresholds were significantly higher at the outer area of our field of view”, explains first author Dr. Wolf Harmening of the University Eye Clinic Bonn, leader of an Emmy-Noether Junior Research Group. “That didn’t come as a surprise. We know that in the periphery of our retina, signals of multiple receptors are combined before they pass later stages in the visual pathway towards the brain. This information convergence is different at and near the center of the retina. For the first time, we are now able to determine this complex interaction at single cell level.”
Better research of eye diseases
Given the new method, expectations for advances in research of eye diseases are high. “Up to now, we were limited to merely observing how retinal structure changes in the progress of a retinal disease”, explains Dr. Harmening. “Now we can take that next step and test cellular function directly, for example by examining whether visual function losses occur before structural changes are observable.” In the past, clinical studies of retinal function had to fully rely on preparations of deceased patients or animal models. Now, possible effects of new medication can be examined more closely and more effectively, since non-invasive experiments can be carried out in the diseased eye directly.
Cutting-edge technology
Stimulating single photoreceptor cells in the living eye is a challenging task. First, the imperfect optics of the human eye and its chromatic dispersive characteristics cause incident light to form a blurry spot on the retina, way too large to hit only a single cell. Second, the human eye is in constant motion, even when steadily fixating, making any retinal location an ever-moving target. These optical hurdles can be compensated by precisely controlling the focus of a laser beam with a deformable mirror, similar to the ones in high-resolution ground-based telescopes. Real-time computer algorithms track eye movement to fire the stimulating laser beam as soon as the target cell is located at the correct position. “By combining these technologies, we ensure stimulation of exactly one cell at a time.”, stresses Dr. Harmening. “It is the only way for individual examination.”
Original Publication: Harmening WM, Tuten WS, Roorda A, Sincich LC. Mapping the Perceptual Grain of the Human Retina. J. Neurosci. 2014 (16): 5667–77. DOI: 10.1523/JNEUROSCI.5191-13.2014
Further information and contact:
Dr. Wolf Harmening
Universitäts-Augenklinik Bonn
Phone: 0228/287-15882
E-mail: wolf.harmening[at]ukb.uni-bonn.de