You are here: vision-research.eu » Vision Research » The Young Researchers View » Miriam Reisenhofer (Q02-2014)
Miriam Reisenhofer and her Research Work
 |
Background
Retinal degenerations severely impair the visual performance and thereby the human social interaction. With more than one million people affected worldwide, Retinitis pigmentosa (RP) is one of the most common retinal degenerative diseases [1].
RP leads to loss of photoreceptor cells, finally causing blindness. A single gene defect is sufficient to cause RP, but to date mutations in over 150 genes have been associated with RP [2], which leads to varying disease phenotypes and makes a therapeutical approach such as gene therapy intricate if not impossible. As there is no neuronal regeneration in the mammalian retina, photoreceptor loss and the subsequent loss of vision is irreversible. So far, several genetically engineered animal models exist to study the disease in vivo. RP pathology, i.e. photoreceptor degeneration, can also be induced by N-methyl-N-nitrosourea (MNU).
MNU has been shown to cause the selective and progressive degeneration of photoreceptors in mice, rats, and non-human primates [3-5]. It is an alkylating agent and leads to a DNA adduct formation in photoreceptor cell nuclei, followed by apoptosis [6]. Although there are differences between the disease development in RP and the mechanism of MNU, the resulting phenotype is comparable [6].
So far, no effective treatment strategy has been found to regain the lost vision in humans. In contrast, non-mammalian vertebrates, like amphibians and fish, have robust regenerative responses to injury, which can lead to near complete restoration of the neurons lost through the injury [7]. This regeneration occurs efficiently from radial glia-type stem/progenitor cells [8]. In the retina of most vertebrates exists only one type of macroglia, the Müller cells [9]. Therefore, investigations of its regenerative properties have been launched in recent years. Thereby, neurogenic changes have been observed in the injured retina, and the source of injury-induced neurogenesis was traced to the Müller cells [10]. Furthermore, it has been shown that purified Müller cells from the rodent display cardinal features of neuronal stem cells in vitro; they self-renew, and, in addition, generate retinal neurons and glia under conducive culture conditions [11].
My Research
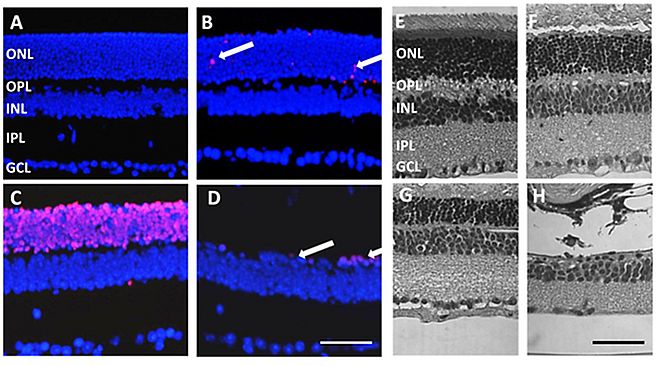
I started my PhD at the Department of Ophthalmology at the Inselspital in Bern, Switzerland, under the supervision of Dr. Volker Enzmann in collaboration with the group of Prof. Andreas Reichenbach at the Paul Flechsig Institute of Brain Research in Leipzig, Germany. In this project, we aim to investigate, whether mammalian Müller cells bear the capacity to serve as an adult stem cell source in the injured retina and can be triggered to dedifferentiate and redifferentiate into the lost cell types. To induce retinal degeneration, mice are treated with MNU. Post treatment, several changes can be observed in the retina. TUNEL positive nuclei appear in the outer nuclear layer (ONL) and the number of cell nuclei in the ONL severely declines. In contrast, the inner nuclear layer (INL) stays intact (Fig. 1).
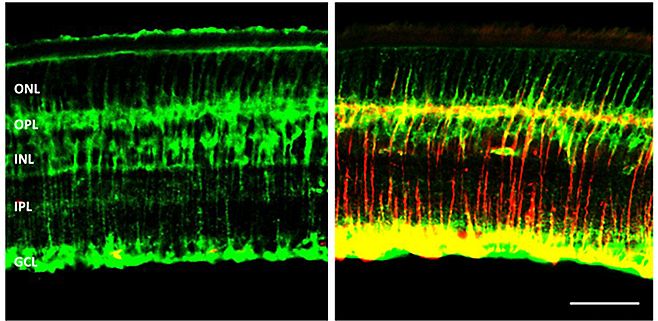
Under physiological conditions, murine Müller cells do not express glial fibrillary acidic protein (GFAP). Upon photoreceptor degeneration, Müller cells are activated and start to express GFAP (Fig. 2).
Furthermore, preliminary analysis of transcription levels shows that progenitor markers (Sox2, Pax6) are transcribed in the degenerating retina, suggesting that Müller cells convert into a stem/progenitor-like cell.
To further characterize the changes of Müller cells in MNU-induced retinal degeneration, I am currently studying electrophysiological properties of Müller cells from MNU-treated animals. It is known from other retinal degenerations (e.g., ischemia [12] or diabetic retinopathy [13]), that rodent Müller cells alter their membrane properties, such as potassium conductance, capacitance or membrane potential.
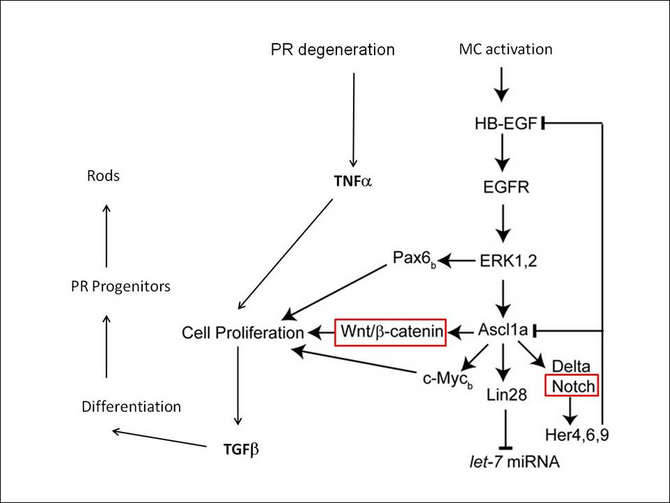
Our goal and future work is to reveal possible pathways (Fig. 3) and mechanisms involved in Müller cell activation and alteration upon photoreceptor degeneration. Key players might be growth factors (EGF, TGFβ) and transcription factors (Ascl1, Pax6) that induce Müller cell proliferation and subsequent differentiation into photoreceptor cells.
Further, we wish to compare our results with findings from the zebrafish, an organism capable of retinal regeneration, to draw conclusions about the capability of mammalian Müller cells to function as an endogenous source for retinal regeneration. Thereby, the MNU model can serve as an useful tool as it induces photoreceptor degeneration in both species and leads to complete regeneration in the zebrafish [15].
References:
- Hartong DT, Berson EL, Dryja TP. Retinitis pigmentosa. The Lancet 2006; 368(9549):1795-1809
- Genes and Mapped Loci Causing Retinal Diseases. Retrieved March 13, 2014, from sph.uth.edu/RetNet/disease.htm
- Nambu H, Nakajima M, Shikata N, Takahashi K, Miki H, Uyama M, Tsubura A. Morphologic characteristics of N-methyl -N-nitrosourea-induced retinal degeneration in C57BL mice. Pathol Int 1997; 47:377–383
- Yoshizawa K, Nambu H, Yang J, Oishi Y, Senzaki H, Shikata N, Miki H, Tsubura A. Mechanisms of photoreceptor cell apoptosis induced by N-methyl-N-nitrosourea in Sprague-Dawley rats. Lab Invest 1999; 79(11):1359-1367
- Tsubura A, Yoshizawa K, Miki H, Oishi Y, Fujii T. Phylogenetic and ontogenetic study of retinal lesions induced by N-Methyl-N-Nitrosourea in animals. Anim Eye Res 1998; 17:97-103
- Tsubura A, Katsuhiko Y, Kiuchi K, Moriguchi K. N-Methyl-N-Nitrosourea-induced Retinal Degeneration in Animals. Acta Histochem Cytochem 2003; 36:263-270
- Karl MO, Reh TA. Regenerative medicine for retinal diseases: activating the endogenous repair mechanisms. Trends Mol Med 2010; 16:193-202
- Kroehne V, Freudenreich D, Hans S, Kaslin J, Brand M. Regeneration of the adult zebrafish brain from neurogenic radial glia-type progenitors. Development 2011; 138:4831-4841
- Reichenbach A, Faude F, Enzmann V, Bringmann A, Pannicke T, Francke M et al. The Muller (glial) cell in normal and diseased retina: A case for single-cell electrophysiology. Ophthalmic Res 1997; 29:326-340
- Bharti K, Miller SS, Arnheiter H. The new paradigm: retinal pigment epithelium cells generated from embryonic or induced pluripotent stem cells. Pigm Cell Res 2011; 24:21-34
- Das AV, Mallya KB, Zhao X, Ahmad F, Bhattachraya S et al. Neural stem cell properties of Müller glia in the mammalian retina: Regulation by Notch and Wnt signaling. Dev Biol 2006; 299:283-302
- Pannicke T, Uckermann O, Iandev I, Biedermann B, Wiedermann P, Perlmann I et al. Altered membrane physiology in Müller glial cells after transient ischemia of the rat retina. Glia 2005; 50:1-11
- Bringmann A, Pannicke T, Grosche J, Francke M, Wiedemann P, Serguei N et al. Müller cells in the healthy and diseased retina. Prog Retin Res 2006; 25:397-424
- Wan J, Ramachandran R, Goldman D. HB-EGF is necessary and sufficient for Muller glia dedifferentiation and retina regeneration. Dev Cell 2012; 22:334-347
- Tappeiner C, Balmer J, Iglicki M, Schuerch K, Jazwinska A, Enzmann V, Tschopp M. Characteristics of Rod Regeneration in a Novel Zebrafish Retinal Degeneration Model Using N-Methyl-N-Nitrosourea. PLoS One 2013; 8(8):e71064
Departement Klinische Forschung - Augenheilkunde
Universität Bern
Universitätsklinik für Augenheilkunde C410a
Inselspital
CH-3010 Bern
Switzerland
Phone: +41 31 632 86 71