You are here: vision-research.eu » Vision Research » Visionary of the Quarter » Andrew Dick (Q01-2021)
Immune regulation: restoring peace
 |
The research work of Professor Andrew D Dick
My move from internal medicine into ophthalmology was driven, in part, by the observation and intrigue that you could see inflammation in the eye. The frustration was soon apparent on how little progress was being made compared to Rheumatology to benefit our patients. Of course, over the decades there has been a progressive understanding of immunity and ocular inflammation, our understanding of tissue immunology and tissue immune homeostasis and all assisted by more refined animal models and ability to interrogate human immunity, through genomics and bioinformatics and environment (microbiome), for example. Complementing this is the contemporary fundamental science and molecular understanding of immune regulation and immune privilege and the break from the stringent paradigms that once purveyed. The drive and hope for me is to deliver a steroid-free life through more targeted therapeutic approaches for the patients with uveitis and developing pathways that may restore immune balance in the eye, thus combatting the devastation of ageing degenerative diseases or facilitating as an adjunct the potential unintended consequences, for example of gene therapy.
Immune regulation reducing Tissue Vulnerability to immune mediated damage
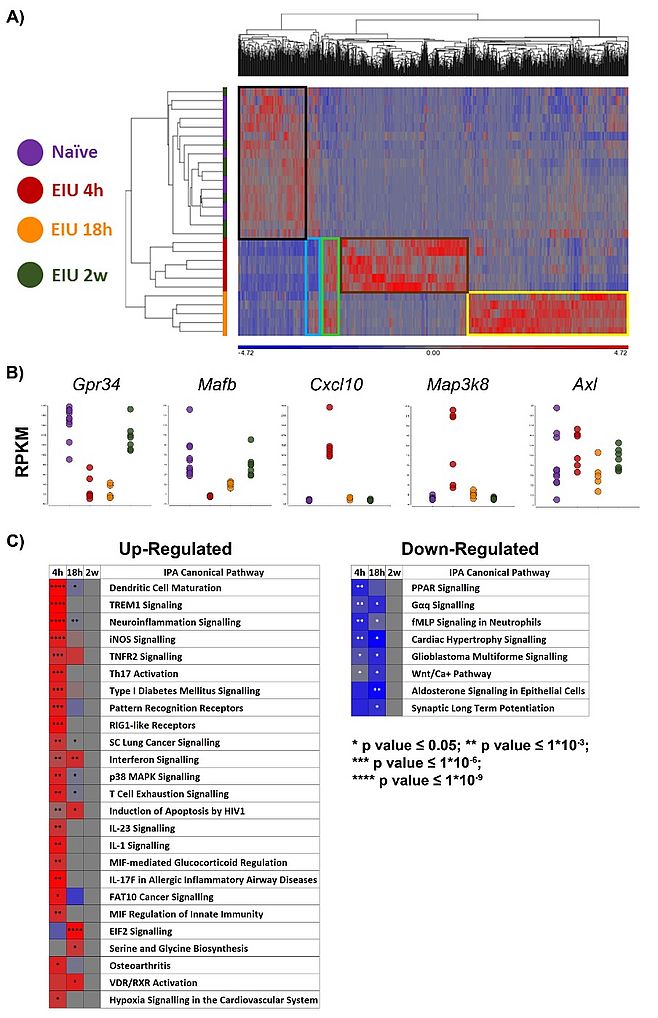
My curiosity has always been, and remains, to understand how the retina sustains function in the majority of us for many years. Despite our fundamental knowledge of how the body, tissues or cells respond to constant danger signals (whether exogenous or endogenous) through and articulate mechanisms of innate immune signals (TLRs etc) or more selective acquisition of memory (adaptive immune responses), there remains the question of how in tissues/organs this protective response does not escalate to promote tissue damage when the immune responses have been activated. The retina (as for all tissues) is constantly immune active and in this context, it possesses many mechanisms to maintain an immune homeostatic environment in response to continuous daily oxidative stress. Yolk-sac derived microglia serve this purpose (although not exclusively). Whilst we and others have shown that microglia are regulated by cognate-receptor interactions, such as CD200R and Cx3CR1 (1-3), which in turn can modulate inflammation in the eye and offer aspects of how therapeutically microglial activation can be regulated to ensure we restore appropriate tissue immunity, the more exciting work now is the understanding of microglial niches and function through RNAseq (Figure 1) (4, 5).
We have demonstrated that Microglia can respond to danger (in this circumstance – TLR4 activation) and return to their active regulatory tissue transcriptome signature. What happens in more chronic conditions has yet to be determined. Similarly, the RPE, whilst not a canonical haemopoietic or yolk sac derived immune cell, is immune competent and provides an outer-retinal immune homeostatic function. Moreover, ageing bring alteration in bio-energetic sourcing within cells (more glycolytic and less mitochondrial), and this is certainly more pronounced under oxidative stress or during activation of immune systems (both observed in age-related macular degeneration). The regulation of immune responses depends on the consequent cellular responses (as seen with IL-33) with how such responses also protect to maintain cell function and sustain mitochondrial health (6, 7).
Personalising therapies for ocular inflammation
Animal models, and particularly the mouse system developed by Rachel Caspi have assisted our understanding of immune pathways in the eye and translating successfully through to man. However, uveitis is an umbrella term of a multitude of different conditions and as a term oversimplifies the complexity of immune pathways and host response. Our earlier work providing evidence of use of immunosuppression in uveitis from mouse to man is limited. Moving on to biologics in the early 1990s with demonstration of the potent ability of CAMPATH-1H (8), we also noted from animal work early on that TNF is a pivotal and orchestrating cytokine (9). Principally (at least in the model) the suppression observed was largely through regulating macrophage and monocyte activation (10) . The experimental potency was upheld with successful translation of TNFi to man and has been arguably transformative for our patients but particularly in children and young people.
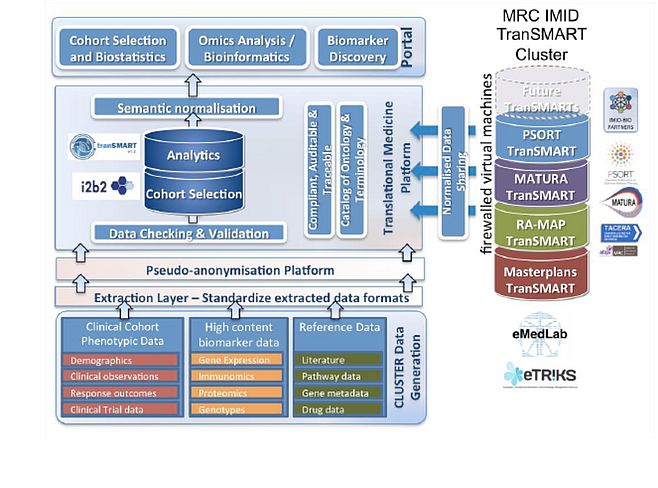
As with all studies, questions arise. Why is the response with TNFi in ‘uveitis’ struggle to get above 65-70%? What was apparent is comparing the blanket coverage of VISUAL Trials for adult uveitis with SYCAMORE trial for JIA-Uveitis (11, 12). SYCAMORE trial was restricted to a ‘single’ phenotype disorder and the data was profound. The trial was terminated early because of the substantial positive effect of TNFi, precluding further placebo use. The benefit has been revolutionary for care of children and young people, with adalimumab now licenced in over 70 countries worldwide. Nevertheless, in this study patients still failed TNFi. To be able to continue our quest to refine our immunomodulatory treatments, we need to understand and focus on molecular patterns of disease and immunity over traditional taxonomy of phenotype and by so doing ‘personalise’ our therapies. As two examples: I am a co-investigator on CLUSTER (led by Professor Lucy Wedderburn at UCL). Cluster’s goal as a consortium between 4 institutions in the UK bringing together disciplines of immunology, clinical, genomic medicine and bioinformatics and artificial intelligence through computer science, is to define in JIA-Uveitis, strata by a distinct functional or pathobiological mechanism or define endotypes (subtypes of a condition characterised by a distinct functional or pathophysiological mechanism). Our hope is that by doing so we will more accurately reflect likely treatment response and disease course as well as illuminate tractable therapeutic pathways (Figure 2). The second, and potentially more immediate, is to refine through clinical trials which patient is most likely to respond. We are commencing this approach in adult uveitis via our ASTUTE RCT in the UK.
Horizon scan from an immunologist’s view
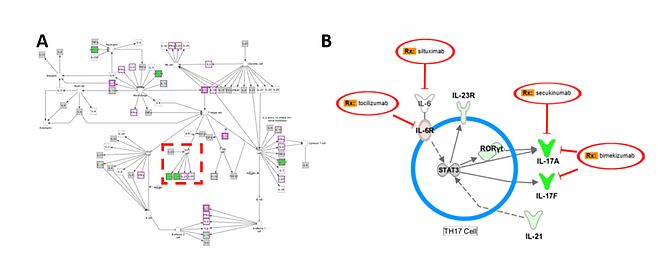
Looking forward, we require to understand pathways and plasticity of immune regulation, immune surveillance and the activated immune response seen in non-infectious uveitis and also across the many chronic disorders that cause immune activation (AMD and Diabetic retinopathy as examples). For immune-mediated inflammatory disorders (IMID), frequently linked to systemic inflammatory disease, we need to unravel the relationship between genes and environment (including microbiome), what makes a tissue vulnerable to attack and lose the immune regulation that keeps the tissue healthy. Within this is the role infectious agents (latent or active) play in initiation or promulgation of IMID (13). To this end and alongside murine systems, we can now interrogate larger patient population cohorts (such as CLUSTER wishes to achieve) to gain insight of the role of individuals genome, environment, tissue responses and outcomes to future stratify our disorders and develop a new taxonomy of disease: that which defines disease by molecular and cellular signature. We can start simultaneously through manipulating the mouse and then define transcriptomic pathways and alternative druggable targets (Figure 3). Together with advances being made in immune imaging (14), afforded by the eye to observe inflammation in real time, I am excited that one of the reasons for the journey from internal medicine to ophthalmology will be realised. As a discipline we can lead future developments of understanding immune responses, novel and personalised treatments for IMID, imaging biomarkers of response, and in roads to treatments of ageing disease through manipulating the immune regulatory networks of the eye.
Acknowledgements
I have been immensely fortunate to work with a tremendous team within the laboratory (figure 4) and in collaboration with many across the globe over many years. A huge thank you to all and for continuing on this exciting journey.
References
- Carter DA, Dick AD. CD200 maintains microglial potential to migrate in adult human retinal explant model. Curr Eye Res. 2004;28(6):427-36.
- Copland DA, Calder CJ, Raveney BJ, Nicholson LB, Phillips J, Cherwinski H, et al. Monoclonal antibody-mediated CD200 receptor signaling suppresses macrophage activation and tissue damage in experimental autoimmune uveoretinitis. The American journal of pathology. 2007;171(2):580-8.
- Dick AD, Broderick C, Forrester JV, Wright GJ. Distribution of OX2 antigen and OX2 receptor within retina. Invest Ophthalmol Vis Sci. 2001;42(1):170-6.
- Bell OH, Copland DA, Ward A, Nicholson LB, Lange CAK, Chu CJ, et al. Single Eye mRNA-Seq Reveals Normalisation of the Retinal Microglial Transcriptome Following Acute Inflammation. Front Immunol. 2019;10:3033.
- O'Koren EG, Yu C, Klingeborn M, Wong AYW, Prigge CL, Mathew R, et al. Microglial Function Is Distinct in Different Anatomical Locations during Retinal Homeostasis and Degeneration. Immunity. 2019;50(3):723-37 e7.
- Clare AJ, Copland DA, Nicholson LB, Liu J, Neal CR, Moss S, et al. Treatment with interleukin-33 is non-toxic and protects retinal pigment epithelium in an ageing model of outer retinal degeneration. J Cell Mol Med. 2020.
- Theodoropoulou S, Copland DA, Liu J, Wu J, Gardner PJ, Ozaki E, et al. Interleukin-33 regulates tissue remodelling and inhibits angiogenesis in the eye. J Pathol. 2017;241(1):45-56.
- Dick AD, Meyer P, James T, Forrester JV, Hale G, Waldmann H, et al. Campath-1H therapy in refractory ocular inflammatory disease. Br J Ophthalmol. 2000;84(1):107-9.
- Dick AD, Forrester JV, Liversidge J, Cope AP. The role of tumour necrosis factor (TNF-alpha) in experimental autoimmune uveoretinitis (EAU). Prog Retin Eye Res. 2004;23(6):617-37.
- Dick AD, McMenamin PG, Korner H, Scallon BJ, Ghrayeb J, Forrester JV, et al. Inhibition of tumor necrosis factor activity minimizes target organ damage in experimental autoimmune uveoretinitis despite quantitatively normal activated T cell traffic to the retina. Eur J Immunol. 1996;26(5):1018-25.
- Jaffe GJ, Dick AD, Brezin AP, Nguyen QD, Thorne JE, Kestelyn P, et al. Adalimumab in Patients with Active Noninfectious Uveitis. N Engl J Med. 2016;375(10):932-43.
- Ramanan AV, Dick AD, Jones AP, McKay A, Williamson PR, Compeyrot-Lacassagne S, et al. Adalimumab plus Methotrexate for Uveitis in Juvenile Idiopathic Arthritis. N Engl J Med. 2017;376(17):1637-46.
- Forrester JV, Kuffova L, Dick AD. Autoimmunity, Autoinflammation, and Infection in Uveitis. Am J Ophthalmol. 2018;189:77-85.
- Joseph A, Chu CJ, Feng G, Dholakia K, Schallek J. Label-free imaging of immune cell dynamics in the living retina using adaptive optics. Elife. 2020;9.

Professor Andrew D Dick
Director of UCL-Institute of Ophthalmology and Duke-Elder Chair of Ophthalmology, UCL, UK.
Professor of Ophthalmology, Bristol Medical School and School of Cellular and Molecular Medicine, University of Bristol, UK.
Theme Lead of Inflammation and Immunotherapeutics, National Institute for Health Research Biomedical Centre Moorfields Eye Hospital UCL Institute of Ophthalmology.
Duke-Elder Chair of Ophthalmology
UCL Institute of Ophthalmology
11-43 Bath Street
London EC1V 9EL
United Kingdom
E-mail: a.dick[at]ucl.ac.uk
Phone: +44 207 608 6808
http:/www.ucl.ac.uk/ioo